This article is written by Dr. Manoj Tiwari.
With the world gripping badly in the fever of COVID-19, different governments are fighting the most devastating war in the history of human civilization to date. It is again proved that nature is Almighty, and we humans (despite all scientific and economic developments) are too helpless in front of the Mother Nature. Yet, humans are known for their fighting spirit and that has resulted in us into the most advanced species on the earth. Right from adopting different procedures (including social distancing, quarantine, and isolations), accelerating researches to develop vaccines, and encouraging the usage of personal protective equipment (PPE) such as masks, gloves, aprons, gowns, and face-shield, etc.; humans are leaving no stone unturned to fight with this pandemic.
1. The Challenge
As per the report of BBC, according to the Department of Health and Social Care (DHSC) in the UK itself 135 million masks, 145 million aprons, 1.2 million gowns, and 470 million pairs of gloves were issued and used from February 25th to April 18th, 2020. This adds to 748 million items used in a span of just 53 days period, making an average 14 million items a day. This is just a glimpse, one can just imagine, the huge numbers of such items being used everyday worldwide. In India alone (who is among the top 10 most suffered nations with COVID-19 as on 28 May 2020), around 200,000 PPE kits are being produced daily in India itself. According to the Government of India sources, the Central government has already distributed about 21.32 lakh PPE kits, and 15.96 lakh kits are kept as a buffer. Further, the total projected demand for PPE kits in India will be around 2.01 crore by the end of June 2020. This all confirms the huge demand for PPE kits to fight against COVID-19.
Now, let’s see the other side of picture. Are we equally serious of safe disposal of used PPE kits (aprons, gowns, gloves, masks, face-shield etc.)? There is a numerous picture in media world-wide where such items are laying on roads or at public places unattended. As these infected (may be infected) items may be a source of further spread of the disease. This issue may bring all the efforts back to square one, if not given immediate and serious attention.
More importantly, as the materials used in most of such items are synthetic materials (which takes hundreds of years in getting decomposed) are becoming the source of pollutions. Just like, plastic bags, these items are laying everywhere on the earth, inside the earth, as well as in the waters (seas and rivers). Such contaminated and infected items are becoming a real threat with each passing day. Only GOD can save us from a new disaster, suppose if such an infected item is consumed by a creature (may be by a cow, pig or may be a fish or a bird) then it may result into a much stronger virus than Corona and may be a question mark on our existence itself..!!!
2. Classification of the waste
We shall discuss the ways to handle the waste of such used items. I hope this may help in sensitizing and educating us towards effective and efficient disposal. Before discussing the disposing procedures, it is important to understand the waste categories. Based on the application, there are two categories of PPE,
- Single use PPE (also called as disposable PPE)
- Reusable PPE.
As name indicates single use PPE should be disposed-off after its use. Many of the PPE used in COVID-19 treatments, such as gloves, masks, overall, shoe protectors etc. fall under this category. Such items should be treated under clinical waste while disposing. Reusable PPE should be treated through an adequate sanitization process (making PPE disinfect), enabling them for reuse.
The Health Technical Memorandum 07-01 (issued by National Health Service - NHS, Department of Health, UK) guides about the best practices and guidelines on Management and disposal of healthcare waste. According to this memorandum, the waste disposal involves a number of activities such as classification and segregation of waste, storage and packaging, transport and treatment of the waste and finally the disposal (NHS, Department of Health, UK, 2013).
As far as the classification is concerned, waste can be classified into two broad categories as clinical waste and offensive waste.
Clinical waste: Any kind of waste is treated as a clinical waste if it may cause infection to any person when coming into contact with it. There may be various sources of clinical waste, few of such sources include medical, veterinary, pharmaceutical, treatment, teaching, research & development etc. A clinical waste may contain human or animal tissue, blood or other body fluids, excretions, drugs or pharmaceutical products, swabs or dressings, syringes, needles or other sharp instruments.
Offensive waste: As name indicates, such waste may cause offence to people (may be due to its appearance or smell). Healthcare and similar municipal waste, apart from clinical wastes may be the sources of such wastes. Nappies, feminine hygiene products, used but uncontaminated PPE (has not been in contact with an infected patient) and incontinence waste are some of the examples of such waste. Most of the times, offensive waste are non-infectious and it does not require specialist treatment or disposal.
3. Handling of the waste
3.1. Doffing PPE
Doffing the PPE is also an important aspect of the context of the spread of infection. It is critical to follow the right sequence of removing PPE from the body. Careful handling while doffing may be the first step toward safety. World Health Organization (WHO) also recommends the sequence of doffing PPE. Please refer to Figure-1 for WHO prescribed doffing sequence of PPE.
Figure-1: Doffing sequence PPE
3.2 Handling the contaminated PPE
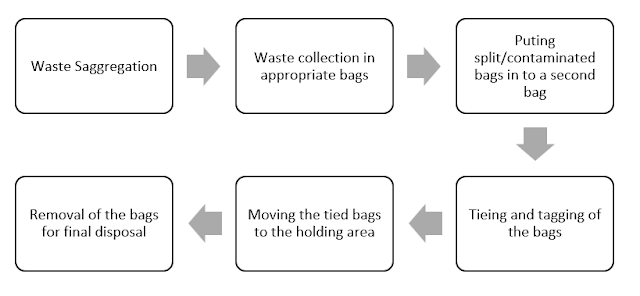
The clinical waste (used infected PPE kits and other related items fall under this category) should be segregated at the source of waste generation. The segregation of waste should be done as per prescribed color coding. Generally, the waste is kept into different containers or bags of specified colors such as blue, orange, transparent, and yellow. There are comprehensive guidelines for waste disposal of each type, but we shall limit our discussion only with the waste from PPE kits as in following steps:
Step 1 : Segregate: Waste items such as PPE used for patient care e.g. (gloves/aprons/masks) should be stored in Orange color bins or bags. The bag should not be full more than its ¾ capacity.
Step 2 : Place: Such contaminated bags should be placed in a second appropriate bag. While handling the clinical waste, the staff should wear appropriate PPE.
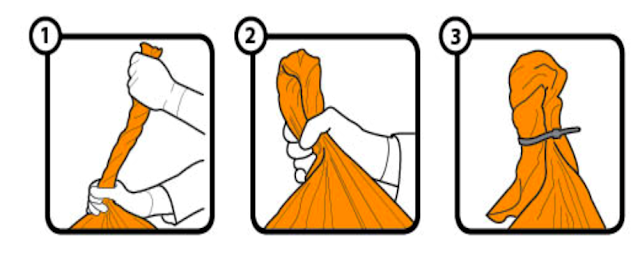
Step 3 : Close: The bags with waste should be tied securely and tagged properly. These bags should also be sealed securely with a suitable plastic tie or secure knot. The recommended method of tying the know is Swan knot (refer figure 2 for Swan knot).
Figure-2: Swan knot
While handling the bags to avoid the infection spread, we must be careful that the bags don’t tear out while moving. We should also check the entire outside surface of the bag for any holes or protruding sharp objects. If there are any holes or protruding sharp objects (such as needles) observed, the bag should be carefully placed inside a larger puncture-resistant container (WHO, 2010). While handling such materials, the workers also follow due safety norms, such as wearing puncture-resistant gloves and face & eye protection to prevent the exposure to such waste streams (infectious materials) (National Waste & Recycling Association, 2020).
The bags should be kept in a locked holding area till further processing when the bags are moved out for final disposal. Refer to Figure-3 for the flow chart of clinical waste handling.
Figure-3: Clinical waste disposal
4. Final disposal of the Waste
Safe rendering (or Render Safe) of clinical waste is an essential requirement. The final disposal should be as per the established practices and norms. The procedural requirements of safe disposal (Render Safe) depend on the type of waste and nature of the contaminants present in the waste (NHS, Department of Health, UK, 2013).
For safe rendering, there are various types of systems available to treat clinical waste. Most of these systems use heat, chemicals, irradiation or combinations of these methods. The clinical waste after rendering should be unusable and unrecognizable. To covert the clinical waste in such a state, both incineration and non-incineration process may be followed. Such processes reduce the chances of waste causing offence. It also eliminates the data confidentiality concerns as well. It is ensured that there is no recognizable clinical waste left after incineration, while in the non-incineration based processes, the clinical waste items are generally macerated (a process of softening with chemical treatment). There are a number of ways available for safe rendering of the clinical waste as mentioned in table 1.
Table-1: Ways of Safe Rendering Clinical waste (NHS, Department of Health, UK, 2013)
|
Category
|
Sub-category
|
Key points
|
|
High temperature processes
|
Incineration
|
Temperature of primary combustion chamber: 800–
1000°C Temperature of secondary combustion chamber:
1100°C (minimum)
Retention time for the combustion gases: 02 seconds
|
|
Pyrolysis
|
Involves high temperature (545– 1000°C) heating
of waste in the absence of oxygen to produce a synthesis gas.
The synthetic gas is mixed with air and combusted
in a secondary chamber at 1100°C temperature.
|
|
Plasma technology
|
Electric current is discharged using an inert
gas to produce a plasma at 6000°C temperature.
Clinical waste is combusted using plasma between
1300– 1700°C temperature.
|
|
Gasification
|
This is similar to the pyrolysis process, but a
small amount of air is used while combustion at a temperature of 900–1100°C.
|
|
Non-burn/low-temperature alternative technologies
|
Heat (thermal) disinfection systems
|
Based on heating the clinical waste to a fixed
temperature for a specified time to deactivate the infectious elements in the
waste.
|
|
Autoclaves
|
Application of
saturated steam (steam holding water as a vapour) is introduced into a vessel
above atmospheric pressure.
|
|
Steam auger
|
Based on thermal disinfection process which operates
at atmospheric pressure with a combination of residence time and temperature treating
the waste and safe render.
|
|
Dry heat
|
Based on the application of electrically generated
heated air, oil or molten plastic.
|
|
Microwaves
|
Based on the combination of the microwaves and
moisture which creates the thermal process results into microbial inactivation.
|
|
Macrowaves
|
Based on the low frequency radio waves for
inactivation of microbes contained in the clinical waste.
|
|
Chemical disinfection systems
|
Based on the chemical treatment to the clinical waste as disinfectants. Most commonly used chemical include sodium hypochlorite,
chlorine dioxide, peracetic acid, glutaraldehyde and quaternary ammonium compounds.
|
|
Other Chemical systems
|
Based on Alkaline Hydrolysis which is a process
for the disposal of clinical waste.
Elevated Pressure with Temperature is kept
around 160°C for 4 to 6 hours. Same results may also be achieved at a lower
pressure and temperature (around 98°C) but takes longer time of around 14 to
16 hours.
|
|
Landfill
|
It is banned to landfill infectious chemical waste.
The chemical waste requires to be pre-treated to make it
non-infectious enabling for landfilling.
|
Conclusion
This article emphasizes the right ways of disposing of the PPE. It is important that the treatment and disposal methods are reliable and consistent in adherence to the prescribed standards. The performance of these methods should be measurable, and the process needs to be controlled. The disposal plants should be audited regularly as per the prescribed guidelines and should have necessary licenses and permits from the respective environment control authority.
To conclude, as a responsible citizen of this earth it is our prime duty to save the environment. The historic war against Corona shall be better justified and successful if we follow the RIGHT Practices and don’t contribute to pollution. This is high time (war against Corona is at its peak, and a large number of PPE are being discarded after use and just left unattended) we must think sensible and act responsibly for a larger cause of saving mother Nature.
References:
- NHS, Department of Health, UK. (2013). Environment and sustainability Health Technical Memorandum 07-01: Safe management of healthcare waste. Department of Health, UK. Crown.
- National Waste & Recycling Association. (2020). COVID 19 Guide for Waste Operations. National Waste & Recycling Association.
- https://www.bbc.com/news/business-52362707
- https://punemirror.indiatimes.com/
- https://www.who.int/
About the Author
Manoj Tiwari
Prof. Manoj Tiwari is affiliated with the Department of Fashion Technology at the National Institute of Fashion Technology, Kannur, India. He earned a Ph.D. from NIFT, Delhi. In addition to teaching, industrial training, research and development, and consulting in India and overseas, he has more than 18 years of professional and academic experience. He served as a Core Team member for the acclaimed INDIAsize project (The National Sizing Survey of India). Know More ...